The mediocre teacher tells. The good teacher explains. The superior teacher demonstrates. The great teacher inspires.
The expert can now integrate his or her grasp of the situation with his or her responses. The expert is able to take up theories and ends of practice in multiple ways, often creating new.
- From Novice to Expert: Exce Several authors have highlighted the role of intuition in expertise. In particular, a large amount of data has been collected about intuition in expert nursing, and intuition plays an important role in the influential theory of nursing expertise developed by Benner 1984.
- The novice to expert model was introduced into nursing by Dr. Patricia Benner in 1982 and discussed how nurses develop skills and understanding of patient care over time (“From novice to expert,” 2013). Benner’s novice to expert model was derived from the Dreyfus Model of Skill Acquisition and adapted to provide a more objective way.
William Arthur Ward
Many of us can relate to the story that Jon Carroll,1 a columnist for the San Francisco Chronicle, tells about his first public singing recital. He had taken a series of singing lessons and then found himself standing on a stage about to sing his first solo in front of a large audience. It took him 4 attempts to find the opening note while he also battled an uncontrollable head bob. Scanning the audience’s faces while he was singing, Carroll said he had the “unshakable perception that cyanide gas had been released in the room and that the face of every person . . . was set in the final rictus of death.” The conclusion of the song was followed by polite applause (the same sort of applause, he wrote, that might occur at the end of a particularly painful 2-hour kettledrum solo). But, to his surprise, his singing teacher walked over to him with tears running down her face and put her arm around him, saying proudly to the audience, “I just want to say that when this man came to me. . .he couldn’t even sing ‘Happy Birthday.’” The audience applauded wildly. Carroll was stunned at the teacher’s remarks and the audience’s reaction. Clearly, this was more than a teacher. She was a mentor. She inspired.
The Need for Nurse Mentors
The nursing profession is in the midst of its longest and most severe shortage. The current shortage has been different from those in past years because of a continuous decline in nursing school enrollments. Causes of this decline include the opening of traditionally male-dominated professions to women, inadequate salary increases in nursing, and nurses speaking out vigorously about their dissatisfaction with the hospital work environment of the 1990s. While fewer people have been seeking nursing careers, the demand for nurses has never been greater (with a projected need for 1 million more nurses by 2010).2 The aging of the baby boomers has created a population growth of elderly or soon-to-be-elderly patients, and advances in healthcare (particularly in our critical care specialty) have led to increasingly complex care.
It appears, however, that the worst of the shortage may now be over, perhaps fueled by a depressed job market and a shortage of places for professional employment. The American Association of Colleges of Nursing reported that nursing school enrollments had risen more than 16% in 2003 compared with the previous year.2 In addition to experiencing an influx of new applicants, nursing schools have adapted their curricula to incorporate accelerated programs and programs for people with baccalaureate degrees in other professions who wish to return to school to study nursing. Although these programs help produce more nurses quickly, they decrease the time devoted to gaining clinical experience. The influx of a substantial number of new nurses into the profession, many of whom may be relatively uninformed about the realities of today’s healthcare system, and the growth of accelerated programs present the next challenge for the critical care team in terms of assimilating these nurses into practice.
From Novice to Expert
In her landmark work From Novice to Expert: Excellence and Power in Clinical Nursing Practice, Dr Patricia Benner3 introduced the concept that expert nurses develop skills and understanding of patient care over time through a sound educational base as well as a multitude of experiences. She proposed that one could gain knowledge and skills (“knowing how”) without ever learning the theory (“knowing that”). Her premise is that the development of knowledge in applied disciplines such as medicine and nursing is composed of the extension of practical knowledge (know how) through research and the characterization and understanding of the “know how” of clinical experience. In short, experience is a prerequisite for becoming an expert. Until publication of Benner’s research, which focused on critical care nurses, this characterization of the learning process had gone largely undefined.
What Does an Expert Nurse Look Like in the Clinical Setting?
Benner used the model originally proposed by Dreyfus4 and described nurses as passing through 5 levels of development: novice, advanced beginner, competent, proficient, and expert. Each step builds on the previous one as abstract principles are refined and expanded by experience and the learner gains clinical expertise.
Instead of seeing patient care as bits of unrelated information and a series of tasks, the expert is able to integrate various aspects of patient care into a meaningful whole. For example, to the novice focusing on mastering the technical aspects of care, an unstable, critically ill postoperative cardiac surgery patient is an urgent to-do list. The vital signs must be noted every 15 minutes, the cardiac rhythm assessed, intravenous drips titrated to keep the blood pressure within a certain range, the lungs auscultated, chest tubes checked routinely, and intake and output recorded.
An expert nurse caring for the same patient would complete the same tasks but not be caught up in the technical details. The expert integrates knowledge of cardiovascular physiology and pathophysiology to assess symptoms and guide patient care; for example, the skin is a little cooler than it should be, the patient is harder to arouse than he was an hour ago, the pulse oximeter shows a decrease in arterial oxygen saturation, and the cardiac monitor shows an irregular heart rhythm. The expert integrates such information and determines that the irregularity is new onset atrial fibrillation and that the cardiac output has probably dropped as a result. The expert knows to watch for emboli, adjust intravenous medications to maintain blood pressure, monitor for other signs and symptoms of reduced cardiac output, and notify the physician about the patient’s change in status. The expert has gone beyond the tasks to read and respond to the whole picture. A potential catastrophe (“failure to rescue” in the lingo of patient safety) is averted.
From Expert to Preceptor
The understanding of what makes an expert nurse has been integral in developing preceptor roles in the intensive care unit (ICU) that help impart this experiential knowledge to nurses new to critical care. The critical care clinician (physician or nurse) makes hundreds of complex decisions each day. It is impossible to teach the myriad circumstances and conditions that a clinician might face daily in the classroom setting or even in a clinical simulation. The clinical expert has a solid technical foundation and the critical thinking skills to adapt to the unique condition of each patient.

Preceptors help new nurses deal with the uncertainty of the clinical setting that is inherent to gaining proficiency. Ultimately, both nursing and medicine are taught in an apprenticeship system, and the role of the “guide at the side” is critical to moving from novice to expert. Imparting knowledge gained by years of experience can be difficult and frustrating for the preceptor and novice alike. The preceptor has learned perceptual distinctions that may be difficult for the novice to understand or the preceptor to teach.
In training experts to be preceptors, facilitators will often use methods that help bring the preceptor back in time to the novice stage. For example, at one local hospital, the instructor responsible for teaching nurses how to be good clinical preceptors brings a musical recorder, an instrument similar to a flute, for each nurse in the class. After giving the class a series of instructions on how to play the recorder, each new clinical preceptor is asked to stand in front of the group and play. This one simple lesson reminds future preceptors what it is like to be a novice and helps them guide new staff nurses skillfully and with empathy.
Inexperienced ICU nurses must deal with a wide variety of complex situations and conditions, many of which they are seeing for the first time. They may feel unsure and vulnerable to being revealed as frauds. Preceptors have to intervene in this potentially lethal situation and give new nurses confidence while carefully monitoring their actions. Being a learner in the challenging environment of an ICU can be difficult, and novice nurses may feel an incredible sense of failure or shame when they make a mistake.
Mentors Wanted
The anticipated influx of new nurses will most likely put demands on current clinical nurse experts and require that they step up into a mentor role for this next generation of nurses. Mentorship has its earliest roots in Homer’s Odyssey written almost 3000 years ago.5 As the story goes, the goddess Athena assumed the role of a nobleman named Mentor in order to teach Telemachus, Odysseus’s son, and to guide him through life’s challenges. Robert Fitzgerald5 correctly refers to Athena’s cognomen in the first book of the Odyssey as “Mentes.” We need talented mentors to guide the next generation of nurses. If the only nurse mentors who apply for the job are those who are long on experience but short on knowledge and skill, we will scare off the next generation!
The concept of a mentor is familiar in the world of business, but more foreign to nursing. Mentors do more than teach skills; they facilitate new learning experiences, help new nurses make career decisions, and introduce them to networks of colleagues who can provide new professional challenges and opportunities. Mentors are interactive sounding boards who help others make decisions.
We like the 5 core competencies of leaders and mentors developed for the Robert Wood Johnson Nurse Fellows Program.6 The first competency is self-knowledge—the ability to understand and develop yourself in the context of organizational challenges, interpersonal demands, and individual motivation. Mentors are aware of their individual leadership strengths and have the ability to understand how others see them. Mentors are also aware of their personal learning styles and are able to work with the different styles of other people.
The second competency is strategic vision—the ability to connect broad social, economic, and political changes to the strategic direction of institutions and organizations. With strategic vision, mentors have the ability to identify key trends in the external environment (eg, reimbursement policies for hospitals, changing roles for men and women, changing patient demographics) and understand the broader impact of the environment on healthcare. With this competency, leaders are able to focus on goals and advise wisely.
The third competency is risk-taking and creativity—mentors have the ability to be successful by moving outside the traditional and patterned ways of success. They are able to identify creative responses to organizational challenges and can tolerate ambiguity and chaos. The mentor is one who develops and sustains creativity and entrepreneurship, encouraging others to take risks and turn mistakes into opportunities for growth.
The fourth competency is interpersonal and communication effectiveness. Great mentors have the ability to nurture a partnership that is mutual and equal, not patriarchal or matriarchal. This skill set requires that mentors be able to give the people they guide a feeling of being included and involved in the relationship. Mentors are great communicators and also great active listeners. They avoid power struggles and dependent relationships and are respectful of the people they guide. They nurture team performance and accountability and give the lifelong gift of confidence.
The fifth competency is inspiration. Mentors are ultimately change-agents who create personal as well as organizational changes. Change is always difficult, and mentors understand and address resistance to change and build teams that can move from planning to action. Mentors encourage change by making others feel hopeful and optimistic about the future. They are able to set a positive and constructive tone and are committed to facilitating growth and career opportunities for others.
The Future of Nursing
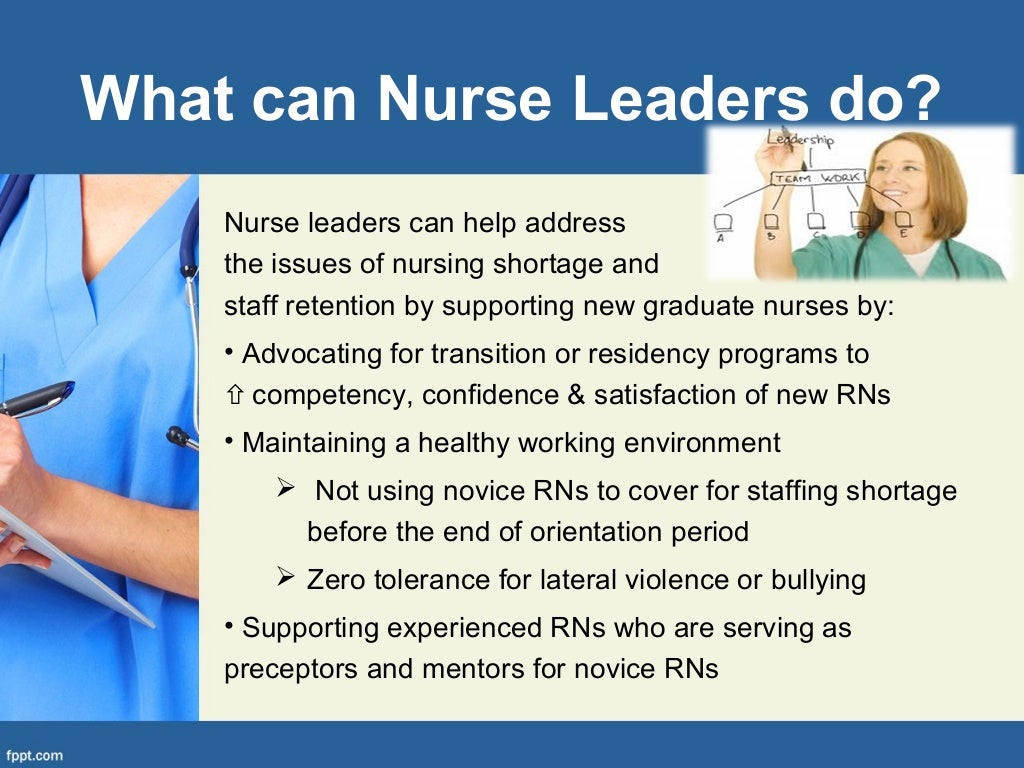
Our opening premise was that we needed to prepare for the challenge of the influx of new nurses at hospitals around the country. Developing preceptor and mentorship programs within our organizations is one effective way to integrate and support the nurses of tomorrow. We need to create these programs if they don’t exist and encourage our colleagues and administrators to support them and participate in them. The acute need for mentors is not a problem that can be solved by nursing alone. Other disciplines can assist with mentoring, and administrators can incorporate incentives for preceptors and mentors, such as salary compensation and career ladder rewards.
With the current influx of new nurses into the profession, we have an opportunity to shape the healthcare system of tomorrow. We can create a system that values talent and generosity of spirit and that rewards professional commitment. Clinical preceptors and career mentors are key to the growth of the nursing profession.
REFERENCES
1Benner From Novice To Expert Pdf 5000
 4
4Footnotes
To purchase reprints, contact The InnoVision Group, 101 Columbia, Aliso Viejo, CA 92656. Phone, (800) 809-2273 or (949) 362-2050 (ext 532); fax, (949) 362-2049; e-mail, reprints@aacn.org.
Seton Hall University Dissertations and Theses (ETDs)
Title
Author
Date of Award
Spring 5-17-2019
Degree Type
Dissertation
Degree Name
PhD Nursing
Department
Nursing
Advisor
Judith Lothian, Ph.D.

Committee Member
Pamela Foley, Ph.D.
Committee Member
Kristi Stinson, Ph.D.
Keywords
Nursing, Disaster Preparedness, Emergency Nursing, Intuition, Triage Decision-Making, New York City
Abstract
Benner From Novice To Expert Pdf 5 Day
Background: Disasters are man-made or natural events that challenge resources and support in an environment lacking rules and regulations. Nurses represent the largest resource in healthcare and are among the first to encounter victims of disaster, thus having knowledge of disaster preparedness is essential to disaster response. However, there is a lack of empirical evidence concerning the relationships between everyday elements of nursing practice such as intuition and triage decision-making and disaster preparedness knowledge.
Purpose: The purpose of this study is to examine the relationships between and among disaster preparedness knowledge, perceived use of intuition, and triage decision-making in emergency department nurses employed in acute care hospitals.
Methods: This descriptive correlational study of one hundred twenty-three emergency department nurses investigated the relationships between and among disaster preparedness knowledge, perceived use of intuition, and triage decision-making in emergency department nurses employed in acute care hospitals in the New York City combined statistical area. Participants completed the following four measurement instruments: The Emergency Preparedness Information Questionnaire, The Acknowledges Using Intuition in Nursing Scale, the Triage Decision Making Inventory, and a Demographic Data Information Form.
Results: Statistical analysis demonstrated that perceived use of intuition and triage decision-making as a group was not predictive of disaster preparedness knowledge. Triage decision-making was predictive of disaster preparedness knowledge by it-self and significant relationships were found between demographic variables related to experience and disaster preparedness knowledge and triage decision-making. Empirical testing of perceived use of intuition demonstrated no significant relationships with disaster preparedness knowledge or triage decision-making.
Conclusion: Emergency department registered nurses will be on the front lines of healthcare’s response to a disaster event. The relationship between disaster preparedness knowledge and triage decision-making suggests that emergency department registered nurses who posses’ higher levels of triage decision-making, have more disaster preparedness knowledge. As such, it is vital that hospital administration, government officials, and professional practice organizations recognize the value of disaster preparedness knowledge and promote innovative methods to educate and train this population of nurses. The empirical evidence of this research study was congruent with Benner’s novice to expert theory indicating that knowledge is gained from previous learning and experience.
Recommended Citation
Schneider, Brian Charles, 'An Investigation of the Relationships Between and Among Disaster Preparedness Knowledge, Perceived Use of Intuition, and Triage Decision Making of Emergency Department Registered Nurses in Acute Care Hospitals Using Benner’s Novice to Expert Theory' (2019). Seton Hall University Dissertations and Theses (ETDs). 2667.
https://scholarship.shu.edu/dissertations/2667
Included in
Critical Care Nursing Commons, Public Health and Community Nursing Commons